Rethinking Industry’s Role in a National Emergency
The shortcomings of the U.S. Strategic National Stockpile must be remedied before the next large-scale public health emergency. Here’s how.
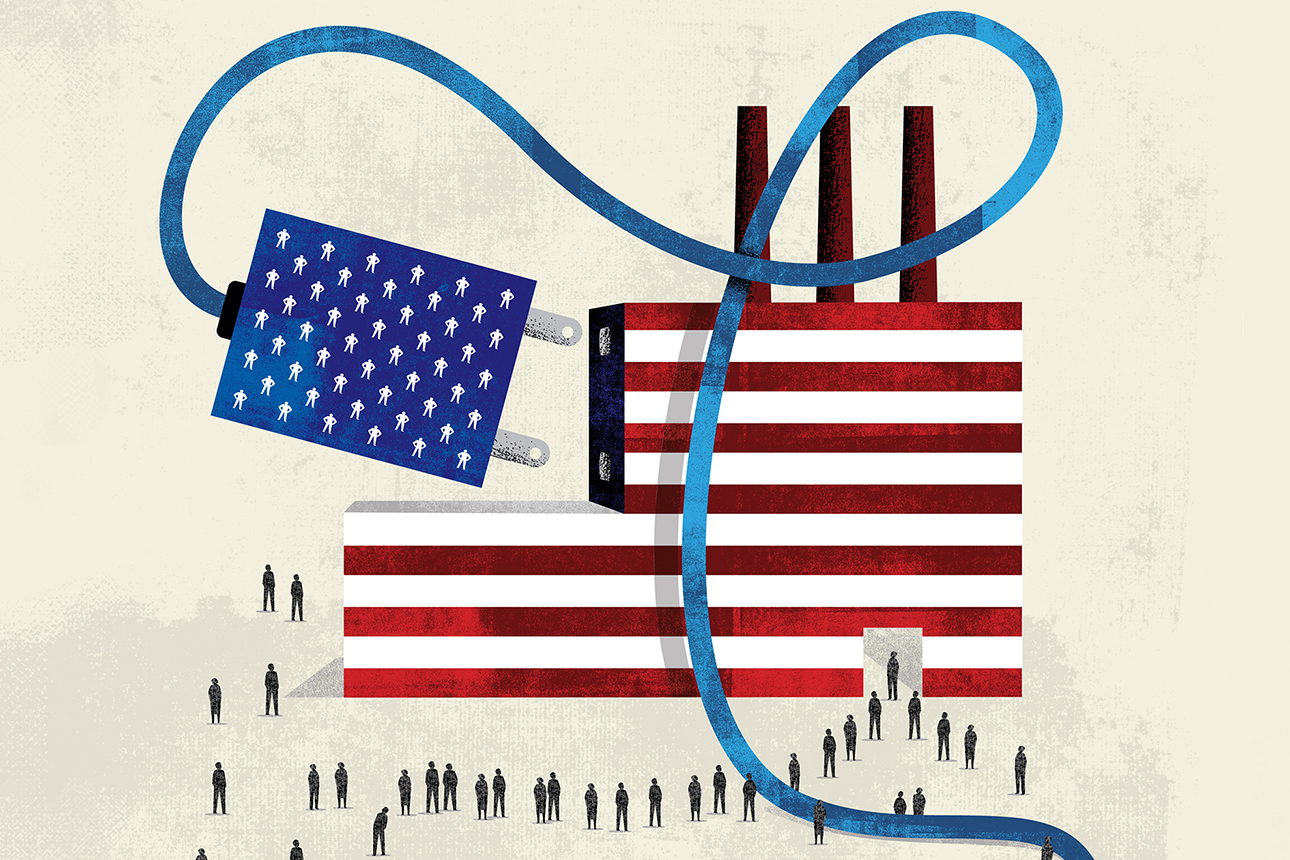
Image courtesy of Michael Austin/theispot.com
Photographs of doctors and nurses wearing garbage bags to protect themselves from infection are among the most indelible images of the COVID-19 pandemic. They also testify to the limitations of the U.S. Strategic National Stockpile (SNS). By the end of March 2020, as the first surge of COVID-19 exceeded 20,000 new cases detected per day, it was woefully clear that the United States’ emergency stockpile of essential medical supplies could not meet the demand for personal protective equipment (PPE), ventilators, and other materials urgently needed to battle the pandemic and save lives.
Since then, there has been plenty of finger-pointing regarding the inability of the SNS to live up to its mandate. But none of that acknowledges the reality that, because of the scale and rarity of pandemic-level public health crises, no national reserve can reliably provide the materials needed from inventory alone.
Get Updates on Transformative Leadership
Evidence-based resources that can help you lead your team more effectively, delivered to your inbox monthly.
Please enter a valid email address
Thank you for signing up
In the decade before COVID-19, flu-related hospitalizations in the U.S. averaged 440,000 annually, but in 2020 alone, COVID-19-associated hospitalizations reached 4.1 million. This is a huge spike in need that is nearly 10 times the flu hospitalization annual mean.1 Moreover, public health emergencies of COVID-19’s magnitude are highly unusual in the U.S. or anywhere else, normally occurring decades apart, which makes the demand spike massive but rare.
After all, the demand challenge for the SNS is to be able to handle the following:
- More severe flus occurring every two to three years, with demand for medical products and equipment being, say, twice the average annual flu hospitalization mean.
- Epidemics and minor pandemics that may occur, say, once every five to 10 years, with demand being as much as three to four times the mean, although the spike may be regional rather than nationwide.
- Severe pandemics occurring once every 20 to 40 years, with demand as high as 10 times the annual mean occurring nationwide.
References
1. “Disease Burden of Influenza,” Centers for Disease Control and Prevention, accessed April 5, 2021, www.cdc.gov; and “Estimated Disease Burden of COVID-19,” Centers for Disease Control and Prevention, accessed April 5, 2021, www.cdc.gov.
2. “SARS Outbreak: Improvements to Public Health Capacity Are Needed for Responding to Bioterrorism and Emerging Infectious Diseases,” PDF file (Washington, D.C.: United States General Accounting Office, May 7, 2003), www.gao.gov; N. Kulish, S. Kliff, and J. Silver-Greenberg, “The U.S. Tried to Build a New Fleet of Ventilators. The Mission Failed,” The New York Times, March 29, 2020, www.nytimes.com; and S.S. Sreshtha, D.L. Swerdlow, R.H. Borse, et. al., “Estimating the Burden of 2009 Pandemic Influenza A (H1N1) in the United States (April 2009-April 2010),” Clinical Infectious Diseases 52, supplement 1 (January 2011): S75-S82.
3. C.R. Wells, M.C. Fitzpatrick, P. Sah, et al., “Projecting the Demand for Ventilators at the Peak of the COVID-19 Outbreak in the USA,” The Lancet Infectious Diseases 20, no. 10 (October 2020): 1123-1125; S. Kliff, A. Satariano, J. Silver-Greenberg, et al., “There Aren’t Enough Ventilators to Cope With the Coronavirus,” The New York Times, March 18, 2020, www.nytimes.com; and R. Branson, J. Dichter, H. Feldman, et al., “The U.S. Strategic National Stockpile Ventilators in Coronavirus Disease 2019: A Comparison of Functionality and Analysis Regarding the Emergency Purchase of 200,000 Devices,” CHEST Journal 159, no. 2 (February 2021): 634-652.
4. Branson et al., “The U.S. Strategic National Stockpile.”
5. Ibid.
6. S. Gompertz and E. Carr, “Coronavirus: Plan to Ramp Up Ventilator Production ‘Unrealistic,’” BBC News, March 16, 2020, www.bbc.co.uk.
7. A. Kobokowich, “Ventilator Stockpiling and Availability in the U.S.,” PDF file (Baltimore, Maryland: Johns Hopkins Center for Health Security, Sept. 3, 2020), www.centerforhealthsecurity.org.
8. G.P. Pisano and W.C. Shih, “Restoring American Competitiveness,” Harvard Business Review 87, no. 7-8 (July-August 2009): 114-125.
9. “Fighting COVID-19 With 3D Printing,” America Makes, accessed April 5, 2021, www.americamakes.us.
10. M.S. Sodhi and C.S. Tang, “Managing Supply Chain Risk” (New York: Springer, 2012).
11. S.G. Stolberg and C. Hamby, “Biden Cancels Visit to Vaccine Maker After Times Report on Its Tactics,” The New York Times, March 8, 2021, www.nytimes.com.
